Between 2000 and 2002 then again from 2008 to 2010 access me
Between 2000 and 2002, then again from 2008 to 2010, access measures showed no improvement and quality of care measures improved more slowly in racial groups and certain ethnic populations, than the improvements for the total population.
Solution
Ans:
The health care quality chasm is better described as a gulf for certain segments of the population, such as racial and ethnic minority groups, given the gap between actual care received and ideal or best care quality. The landmark Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century challenges all health care organizations to pursue six major aims of health care improvement: safety, timeliness, effectiveness, efficiency, equity, and patient-centeredness. “Equity” aims to ensure that quality care is available to all and that the quality of care provided does not differ by race, ethnicity, or other personal characteristics unrelated to a patient\'s reason for seeking care. Baylor Health Care System is in the unique position of being able to examine the current state of equity in a typical health care delivery system and to lead the way in health equity research. Its organizational vision, “culture of quality,” and involved leadership bode well for achieving equitable best care. However, inequities in access, use, and outcomes of health care must be scrutinized; the moral, ethical, and economic issues they raise and the critical injustice they create must be remedied if this goal is to be achieved. Eliminating any observed inequities in health care must be synergistically integrated with quality improvement. Quality performance indicators currently collected and evaluated indicate that Baylor Health Care System often performs better than the national average. However, there are significant variations in care by age, gender, race/ethnicity, and socioeconomic status that indicate the many remaining challenges in achieving “best care” for all.
Explanation: The U.S. health care system is designed to improve the physical and mental well-being of all Americans by preventing, diagnosing, and treating illness and by supporting optimal function. Across the lifespan, health care helps people stay healthy, recover from illness, live with chronic disease or disability, and cope with death and dying. Quality health care delivers these services in ways that are safe, timely, patient centered, efficient, and equitable.
Unfortunately, Americans too often do not receive care they need, or they receive care that causes harm. Care can be delivered too late or without full consideration of a patient\'s preferences and values. Many times, our system of health care distributes services inefficiently and unevenly across populations. Some Americans receive worse care than others. These disparities may occur for a variety of reasons, including differences in access to care, social determinants, provider biases, poor provider-patient communication, and poor health literacy.
Each year since 2003, the Agency for Healthcare Research and Quality (AHRQ) has reported on progress and opportunities for improving health care quality and reducing health care disparities.
As per the 2012 NHQR and NHDR: This is intended to reinforce the need to consider concurrently the quality of health care and disparities across populations when assessing our health care system. The National Healthcare Reports Highlights seek to address three questions critical to guiding Americans toward the optimal health care they need and deserve:
Three themes from the 2012 NHQR and NHDR emphasize the need to accelerate progress if the Nation is to achieve higher quality and more equitable health care in the near future:
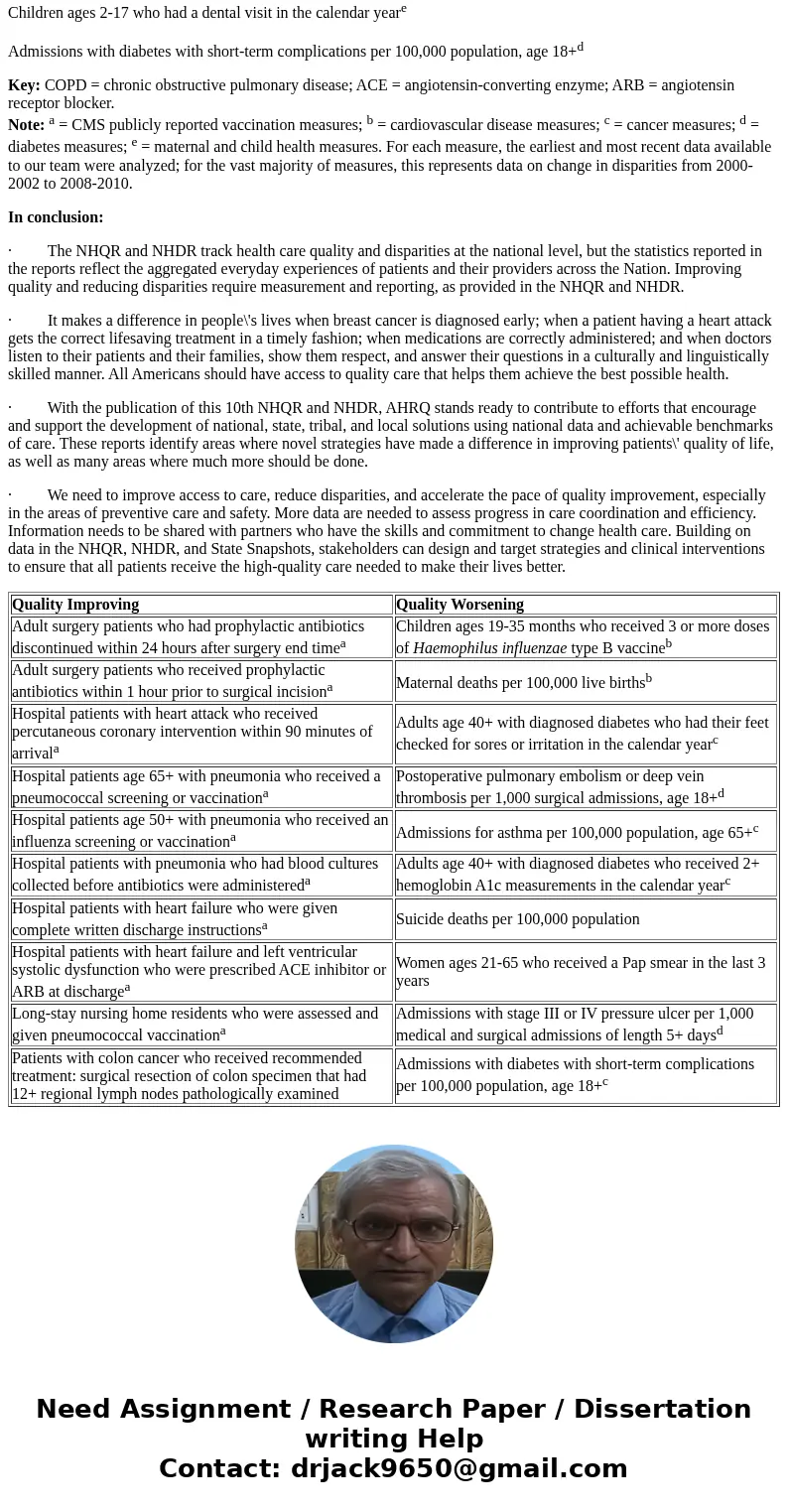
Quality measures with the most rapid pace of improvement and deterioration
Quality Improving
Quality Worsening
Adult surgery patients who had prophylactic antibiotics discontinued within 24 hours after surgery end timea
Children ages 19-35 months who received 3 or more doses of Haemophilus influenzae type B vaccineb
Adult surgery patients who received prophylactic antibiotics within 1 hour prior to surgical incisiona
Maternal deaths per 100,000 live birthsb
Hospital patients with heart attack who received percutaneous coronary intervention within 90 minutes of arrivala
Adults age 40+ with diagnosed diabetes who had their feet checked for sores or irritation in the calendar yearc
Hospital patients age 65+ with pneumonia who received a pneumococcal screening or vaccinationa
Postoperative pulmonary embolism or deep vein thrombosis per 1,000 surgical admissions, age 18+d
Hospital patients age 50+ with pneumonia who received an influenza screening or vaccinationa
Admissions for asthma per 100,000 population, age 65+c
Hospital patients with pneumonia who had blood cultures collected before antibiotics were administereda
Adults age 40+ with diagnosed diabetes who received 2+ hemoglobin A1c measurements in the calendar yearc
Hospital patients with heart failure who were given complete written discharge instructionsa
Suicide deaths per 100,000 population
Hospital patients with heart failure and left ventricular systolic dysfunction who were prescribed ACE inhibitor or ARB at dischargea
Women ages 21-65 who received a Pap smear in the last 3 years
Long-stay nursing home residents who were assessed and given pneumococcal vaccinationa
Admissions with stage III or IV pressure ulcer per 1,000 medical and surgical admissions of length 5+ daysd
Patients with colon cancer who received recommended treatment: surgical resection of colon specimen that had 12+ regional lymph nodes pathologically examined
Admissions with diabetes with short-term complications per 100,000 population, age 18+c
Key: ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker.
Note: a = CMS publicly reported measures; b = maternal and child health measures; c = diabetes measures; d = adverse events. For each measure, the earliest and most recent data available to our team were analyzed; for the vast majority of measures, this represents trend data from 2000-2002 to 2008-2010.
Table H.2. Disparities that are changing over time
Groups
Disparities Improving
Disparities Worsening
Black compared with White
Admissions for congestive heart failure per 100,000 population, age 18+b
Advanced stage invasive breast cancer incidence per 100,000 women age 40+c
Adjusted incidence of end stage renal disease due to diabetes per million populationd
Maternal deaths per 100,000 live birthse
Short-stay nursing home residents who were assessed and given pneumococcal vaccinationa
Asian compared with White
Hospital patients age 65+ with pneumonia who received a pneumococcal screening or vaccinationa
Adjusted incidence of end stage renal disease due to diabetes per million populationd
Hospital patients age 50+ with pneumonia who received an influenza screening or vaccinationa
Hospice patients who received the right amount of help for feelings of anxiety or sadness
Hospital patients with heart failure who were given complete written discharge instructionsb
Adults ages 18-64 at high risk (e.g., COPD) who ever received pneumococcal vaccination
American Indian/ Alaska Native compared with White
Adjusted incidence of end stage renal disease due to diabetes per million populationd
Hospital patients with heart failure and left ventricular systolic dysfunction who were prescribed ACE inhibitor or ARB at dischargeb
Children who had their height and weight measured by a health provider within the past 2 yearse
Adults age 50+ who ever received a colonoscopy, sigmoidoscopy, or proctoscopyc
Hispanic compared with Non-Hispanic White
Admissions for congestive heart failure per 100,000 population, age 18+b
Home health care patients who have less shortness of breath
Hospital patients age 65+ with pneumonia who received a pneumococcal screening or vaccinationa
Adults age 40+ with diagnosed diabetes who received 2+ hemoglobin A1c measurements in the calendar yeard
Hospital patients age 50+ with pneumonia who received an influenza screening or vaccinationa
Hospital patients with heart attack who received fibrinolytic medication within 30 minutes of arrivalb
Poor compared with High Income
Admissions for congestive heart failure per 100,000 population, age 18+b
People without a usual source of care who indicate a financial or insurance reason for not having a source of care
Deaths per 1,000 hospital admissions with abdominal aortic aneurysm repair, age 18+b
Adults age 50+ who ever received a colonoscopy, sigmoidoscopy, or proctoscopyc
Children ages 2-17 who had a dental visit in the calendar yeare
Admissions with diabetes with short-term complications per 100,000 population, age 18+d
Key: COPD = chronic obstructive pulmonary disease; ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker.
Note: a = CMS publicly reported vaccination measures; b = cardiovascular disease measures; c = cancer measures; d = diabetes measures; e = maternal and child health measures. For each measure, the earliest and most recent data available to our team were analyzed; for the vast majority of measures, this represents data on change in disparities from 2000-2002 to 2008-2010.
In conclusion:
· The NHQR and NHDR track health care quality and disparities at the national level, but the statistics reported in the reports reflect the aggregated everyday experiences of patients and their providers across the Nation. Improving quality and reducing disparities require measurement and reporting, as provided in the NHQR and NHDR.
· It makes a difference in people\'s lives when breast cancer is diagnosed early; when a patient having a heart attack gets the correct lifesaving treatment in a timely fashion; when medications are correctly administered; and when doctors listen to their patients and their families, show them respect, and answer their questions in a culturally and linguistically skilled manner. All Americans should have access to quality care that helps them achieve the best possible health.
· With the publication of this 10th NHQR and NHDR, AHRQ stands ready to contribute to efforts that encourage and support the development of national, state, tribal, and local solutions using national data and achievable benchmarks of care. These reports identify areas where novel strategies have made a difference in improving patients\' quality of life, as well as many areas where much more should be done.
· We need to improve access to care, reduce disparities, and accelerate the pace of quality improvement, especially in the areas of preventive care and safety. More data are needed to assess progress in care coordination and efficiency. Information needs to be shared with partners who have the skills and commitment to change health care. Building on data in the NHQR, NHDR, and State Snapshots, stakeholders can design and target strategies and clinical interventions to ensure that all patients receive the high-quality care needed to make their lives better.
| Quality Improving | Quality Worsening |
| Adult surgery patients who had prophylactic antibiotics discontinued within 24 hours after surgery end timea | Children ages 19-35 months who received 3 or more doses of Haemophilus influenzae type B vaccineb |
| Adult surgery patients who received prophylactic antibiotics within 1 hour prior to surgical incisiona | Maternal deaths per 100,000 live birthsb |
| Hospital patients with heart attack who received percutaneous coronary intervention within 90 minutes of arrivala | Adults age 40+ with diagnosed diabetes who had their feet checked for sores or irritation in the calendar yearc |
| Hospital patients age 65+ with pneumonia who received a pneumococcal screening or vaccinationa | Postoperative pulmonary embolism or deep vein thrombosis per 1,000 surgical admissions, age 18+d |
| Hospital patients age 50+ with pneumonia who received an influenza screening or vaccinationa | Admissions for asthma per 100,000 population, age 65+c |
| Hospital patients with pneumonia who had blood cultures collected before antibiotics were administereda | Adults age 40+ with diagnosed diabetes who received 2+ hemoglobin A1c measurements in the calendar yearc |
| Hospital patients with heart failure who were given complete written discharge instructionsa | Suicide deaths per 100,000 population |
| Hospital patients with heart failure and left ventricular systolic dysfunction who were prescribed ACE inhibitor or ARB at dischargea | Women ages 21-65 who received a Pap smear in the last 3 years |
| Long-stay nursing home residents who were assessed and given pneumococcal vaccinationa | Admissions with stage III or IV pressure ulcer per 1,000 medical and surgical admissions of length 5+ daysd |
| Patients with colon cancer who received recommended treatment: surgical resection of colon specimen that had 12+ regional lymph nodes pathologically examined | Admissions with diabetes with short-term complications per 100,000 population, age 18+c |
 Homework Sourse
Homework Sourse